Dr. Pojer is president of the OGKA (Austrian Society for Controlled Acupuncture and TCM) and an academic at the Medical University of Graz (Austria). She has written a post based on the topic of her new book Integrative Treatment of Male Infertility with Chinese Medicine.
On average one out of six European couples experience sub/infertility. Looking at the reasons for unfulfilled parenthood, approximately 50 percent are due to female pathology and 50 percent are due to male issues. However, society as well as medicine (both Western and Eastern approaches) tends to focus on treating the female side of childless couples. Since the percentage of male factor infertility is the same as that for female infertility, treatment of the male partner is underrepresented. The overall sperm quality has dropped by 50% within the last 40 years but additionally, the COVID pandemic has aggravated the problem. On top of this, the male factor plays an important role in early pregnancy loss and should be treated to prevent miscarriage.
The Covid-19 virus dramatically reduced almost every parameter tested in a standard semen analysis. The infection not only impairs sperm quality but also diminishes testosterone levels. That might be one of the commonly unknown side effects of the pandemic, yet hardly anyone is aware of it, but it is relevant for every man. Chinese Medicine has a lot to offer to improve overall male health.
In an integrative aspect, it is important to know that with Chinese Medicine treatment time, one has to stick to a timeline according to the physiological sperm development. That is a perfect example of why it is essential even as a Chinese Medicine practitioner to know plenty about Western Medicine physiology and pathology of the male reproductive tract. If you know how it should work, you´ll know what to do and when to treat it if it doesn´t work properly!
Sperm development starts in the testes and takes roughly 64 days, during which the process can be disturbed by many external and internal influences. After 64 days of development in the testes, sperm move to the epididymis to mature in terms of motility and functionality, which takes another 8 to 14 days. Therefore, sperm production lasts approximately 72 days altogether. This knowledge should inform the Chinese medicine treatment plan. It means that the male partner typically needs a minimum of 72 days of treatment prior to conception (whether natural or using artificial reproductive technologies [ART]) to improve his sperm parameters. This is something that needs to be discussed with male patients to assure they will stick to the treatment plan.
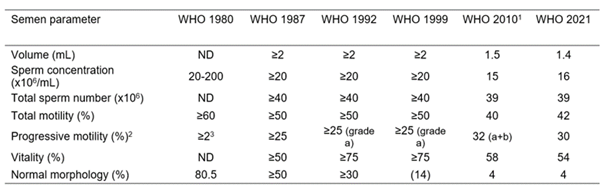
Talking about sperm quality, let´s have a look at the common parameters tested. Semen analysis (according to the new WHO 6th edition 2021) includes the following:
- ‘Volume’, ‘concentration’ and ‘total sperm count’ represent the total volume of the ejaculation and its contents in terms of sperm cells. A normal volume is 1.4 millilitres or greater. The volume may be low if a man is anxious when producing a specimen, if all of the semen is not caught in the collection container, or if there are hormonal abnormalities or ductal blockages. In terms of concentration, each millilitre of semen should contain 2 to 16 million sperm cells. Total sperm count is calculated by multiplying the sperm concentration by the ejaculate volume and should be more than 39 million
- The pH of semen should be slightly alkaline (7.2 or greater)
- Motility is divided into three categories: forward progression (so-called ‘forward swimmers’), non-progressive motility (i.e. ‘swimming in circles’) and immotility. Motility is considered to be normal if at least 40 percent can move at all (i.e. total motility – including both forward and non-progressive swimmers) and 30 percent can move progressively forward
- Morphology: The minimum level of normal forms is 4 percent (this dropped from 14 percent in the stricter pre-2010 guidelines)
What is the role of Chinese Medicine when it comes to boosting sperm quality?
First of all, lifestyle changes have to be made as many environmental, dietary, and lifestyle ´sins´ have a huge impact on sperm quality. Advising our patients to live healthier has always been something Chinese Medicine practitioners have been great at. So gain knowledge in what impacts male fertility and spread it among your patients.
Secondly, out of our Chinese medical toolbox, acupuncture is helpful to improve sperm quality as it improves blood flow to the testicles, lowers and clears infections and reduces oxidative stress.
Here are some examples of research on that topic, you might want to know about:
- Sperm morphology: Forty men with idiopathic oligospermia, asthenospermia, or teratozoospermia were randomised to an acupuncture group (n=28), who received acupuncture twice a week over a period of 5 weeks, and a control group (n=12) who were untreated. Primary points used were Guanyuan REN-4, Ciliao BL-32, Taichong LIV-3, Taixi KID-3; secondary points included Zusanli ST-36, Xuehai SP-10, Sanyinjiao SP-6, Guilai ST-29 and Baihui DU-20. After treatment, there was a statistically significant increase in the percentage and number of sperm without structural defects1
- Sperm count and motility: A total of 121 patients diagnosed with oligozoospermia, asthenozoospermia or oligoasthenozoospermia were randomised into four groups. Patients in the treatment groups were treated with transcutaneous electrical acupuncture point stimulation at different frequencies: 2Hz (n=31), 100Hz (n=31) or mock stimulation (n=29) at acupuncture points Shenshu BL-23, Zusanli ST-36, Huiyin REN-1,Shenshu BL-23 and Guanyuan REN-4 for 2 months. The control group (n=30) was provided with lifestyle advice only. Significant changes in total sperm count and motility were found in the 2 Hz group compared to the controls2
Thirdly Chinese herbs have a proven effect on different parameters tested in a semen analysis. They often work via harmonizing the hormones of the hypothalamic-pituitary-testis axis and so have an impact on certain cell types in the testicles, improving sperm development.

The hypothalamic-pituitary-testicular (H-P-T) axis is a major positive- and negative-endocrine feedback system that regulates testis function. Hormone levels that are either too high or too low are detrimental to spermatogenesis.
Modern research has demonstrated that e.g. kidney deficiency often manifests with the dysfunction and impaired structure of the H-P-T axis
Here are some research results that you might want to know about:
Enhancement of follicle-stimulating hormone levels, regulation of luteinizing hormone level
Low levels of FSH imply hypospermatogenesis. Kidney-supplementing and replenishing herbal medicines heightened testicular function in spermatogenesis through upregulation of FSH:
- Go Qi Zi (Lycium barbarum): could significantly raise FSH and LH levels3
- Ren Shen (Ginsenoide): Ginsenosides were able to stimulate cultured anterior pituitary cells to secrete FSH and LH in vitro4
- Liu Wei Di Huang Wan significantly increased FSH and LH levels in kidney–yin–deficient infertile men5
- Wu Zi Yan Zong Wan promotes the secretion of FSH and to simultaneously reduces LH levels through a negative feedback pathway6
If you want to know more, I’ll warmly invite you to meet Sam the Sperm:

and Professor Sperm
They lead you through my book and help you gain knowledge on how to improve male fertility from a Chinese Medicine perspective but also a Western Medicine one.
Integrative Treatment of Male Infertility with Chinese Medicine is available for pre-order now.
If you liked this article, why not join our mailing list to receive exclusive content and discounts? Sign up to the mailing list here
1 Pei, J., Strehler, E., Noss, U., Abt, M. et al. (2005). Quantitative evaluation of spermatozoa ultrastructure after acupuncture treatment for idiopathic male infertility, Fertility and Sterility, 84, 1, pp. 141-7.
2 Yu, Y., Sha, S., Zhang, B. et al. (2019). Effects and mechanism of action of transcutaneous electrical acupuncture point stimulation in patients with abnormal semen parameters, Acupunct Med., 37, 1, pp. 25-32
3 (Luo Q, Li Z, Huang X, Yan J, Zhang S, Cai YZ. Lycium barbarum polysaccharides: protective effects against heat-induced damage of rat testes and H2O2-induced DNA damage in mouse testicular cells and beneficial effect on sexual behavior and reproductive function of hemicastrated rats. Life Sci. 2006;)
4 *(Li X, Liu S, Ma X, Xu J. A study of the effect of ginsenosides on the secretion of gonadotropins. J Norman Bethune Univ Med Sci. 1988;14:293–295)
5 (*Ye Z, Chen D, Zhong J, Zhang Y, Zhang W, Wang G, et al. Effect of Jiawei Wuzi Yanzong decoction on sperm quality and hormone level. World Chin Med., 2013)
6 (Xie J, Wang J, Chen M, Liu H. Influence of Guilingji capsules on spermatogenesis and sexual hormones in oligospermatism rats. J Guangzhou Univ Tradit Chin Med., 2011)