Written by Isobel Knight
On 22-4-22 I had the honour of being interviewed by Kerry Gabrielson who runs a Podcast series called, ‘Hypermobility Happy Hour‘. The interview assumes some knowledge on the topic of hypermobility, heritable connective tissue disorders especially the ‘hypermobile Ehlers-Danlos Syndrome’ – the one and most common subtype of a total of 13 different (much rarer) types of Ehlers-Danlos Syndrome (EDS). The other condition much referred to is Hypermobility Spectrum Disorder (HSD), which is the resultant diagnosis if one has symptomatic hypermobility and doesn’t meet the (2017) criterion of hEDS. So what do these terms mean in lay-terms?
What is meant by Hypermobility?
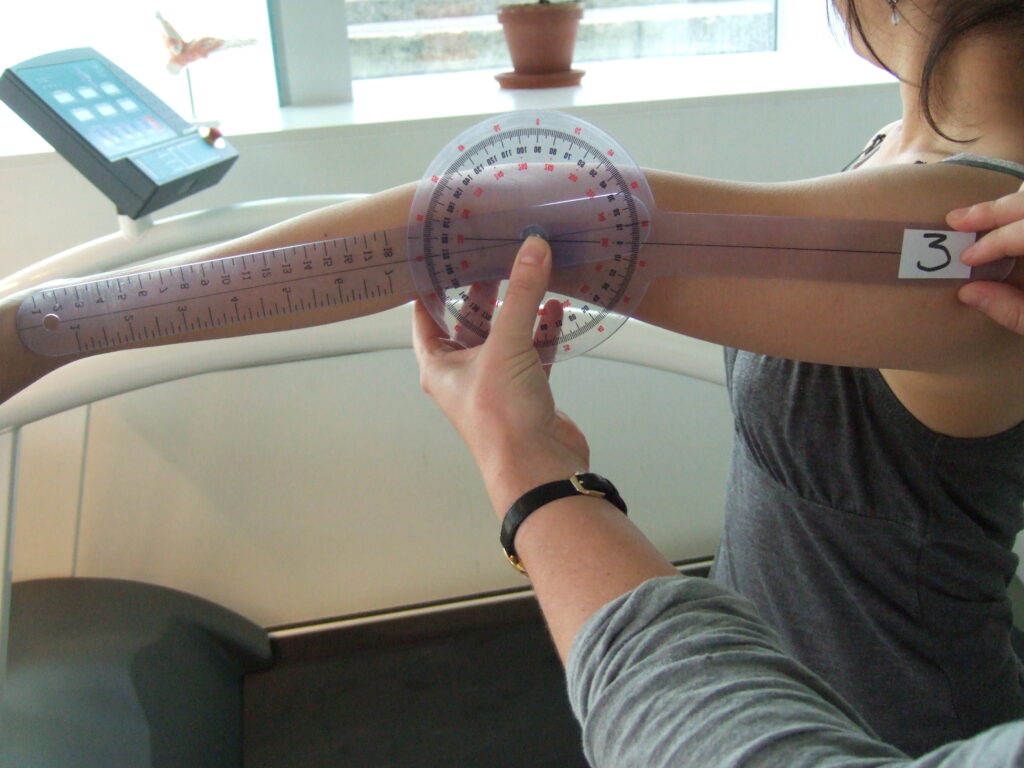
A hypermobile joint is one with a greater than average range of movement when observed by eye, or more accurately with a Goniometer (Figure 1). An observed hypermobile joint might look inside out for example, and a joint that is passively hyper-extended in excess of 10 degrees when measured with a Goniometer would be considered hypermobile. It is certainly possible to have generalised hypermobility of joints and not have any difficulties or problems with the joints, and that is known as generalised joint hypermobility (GJH). It seems that most people have an awareness of their hypermobility, or ‘being loose jointed’.
Being hypermobile without any symptoms is certainly possible, and it is very common in the dance, performing arts and sports world. It can be an asset when it is not causing pain or problems. However, it ceases to be an asset when pain and symptoms prevail.
hypermobile Ehlers-Danlos Syndrome – hEDS
When a person has symptomatic hypermobility – that is, that it causes pain and other symptoms; it might be considered to be a Heritable Disorder of Connective Tissue (HDCT). We are covered in connective tissues – that affect collagen fibres and fibrous protein genes. It is the faulty genes that cause a HDCT. People with hEDS frequently look healthy, and yet through their faulty genes and collagens they are subject to soft, velvety and fragile papery skin that is often easily bruised. Their faulty collagens and altered connective tissue affect their joints leading to ‘ligamentous laxity’ and the hypermobility then causes problems possibly even dislocations of joints, soft-tissue trauma and frequent, easy musculoskeletal injuries. Pain is never far away, and muscles are often in spasm at the helm of trying to overwork and control the lax and loose ligaments that are over-stretched and do not hold the joints as well as they should. People who are hypermobile often have what is known as poor proprioception. The term proprioception is a sixth sense and helps us to have an awareness of where we are in space. In those with hypermobility (symptomatic or asymptomatic), proprioception can be impaired. For those who are naturally hypermobile and asymptomatic, as well as those who are, both need to work at strengthening their joints and surrounding tissues – so physiotherapy/PT is important for those who have hypermobility – especially if they have HDCT and the condition Ehlers-Danlos Syndrome, which is also related to other soft connective tissue conditions such as Marfan Syndrome, Osteogenia Imperfecta.
There are 13 types of EDS and one is particularly serious- the vascular type – vEDS as this can lead to fragility of the vascular damage and vascular tears can be very dangerous to the blood vessels in this subtype. All except for the hypermobile EDS -hEDS have known genetic tests and genotypes, but at the moment we don’t yet know the genetic combination for hEDS, the most common type of EDS and/or Hypermobility Spectrum Disorder (HSD).
In addition to the skin and musculoskeletal system, there are other conditions that affect the connective tissue – the bowel, for example, is made up of connective tissues, as are the lungs and blood vessels, the bladder is made up of connective tissues. They are found everywhere in the body, so that nearly every bodily system might be affected with EDS.
There are other conditions that are associated with both hEDS and HSD such as Postural orthostatic Tachycardia Syndrome (PoTS) – that strongly impacts upon the autonomic nervous system, which has branches known as the Sympathetic Nervous System (SNS) sometimes called ‘fight and flight’ and the Parasympathetic Nervous System (SNS), that is known as ‘rest and digest’. People with PoTS often suffer from tachycardia (fast heart rate), heat intolerance, sweating, blood pressure disturbance, fainting, bladder, bowel problems and more. In addition the gastrointestinal system is often badly affected in patients with hEDS and HSD, and panic and anxiety has a well established link, and is very common. Neurodivergent conditions such as Autism Spectrum Disorder (ASD), Development Coordination Disorder (DCD) and other Neurodivergent conditions have been shown to have associations with hEDS and HSD.
However the 2017 diagnostic criteria have very stringent markers that mean only hypermobility with skin symptoms, close family relatives with hEDS (genetics) and pain in general, are definite aspects of diagnosis, as well as excluding other types of HDCT (such as Marfan Syndrome). Those who do not make all these criteria may be given the diagnosis of Hypermobility Spectrum Disorder -HSD. However, the management of both conditions should be very similar and each treated with the same level of importance.
As I write, the 2017 diagnostic criteria for both hEDS and HSD are being revised and the outcome of this research will become public sometime during 2024. This is exciting news for everyone. Research is going on into all HDCTs all the time. What we do know is that hEDS and HSD are not rare, just rarely diagnosed. Again, hopefully the speed of diagnosis will improve as awareness of these conditions continue to grow, and awareness increases amongst the medical profession.
Hypermobility Spectrum Disorder
Formerly known as Joint Hypermobility Syndrome (JHS), the term HSD was introduced in 2017 in response to improved research criteria and tightening the diagnosis for hEDS so that those who did not meet the new hEDS criteria might instead have the diagnosis of HSD which should be just as valid as a diagnosis of hEDS – but people might be on varying stages of the spectrum with HSD – just as they might be for Autism Spectrum Disorder (ASD), and managed accordingly. However, some patients have been upset with the apparently lesser condition of HSD – but as I mentioned earlier both hEDS and HSD should be managed in a very similar manner. The other new thing in the HSD are that there are different types of hypermobility put into subtypes – for example there is Peripheral Hypermobility that might affect the joints of the hands and feet, whilst Historical Hypermobility refers to hypermobility that someone had when they were younger, as hypermobility should, theoretically decrease with age. Generalized joint hypermobility is where hypermobility is found in wider joints such as the knees, elbow and spine. Again, it is possible to be hypermobile and asymptomatic – think of dancers, musicians and performing artists, whereas those affected will be on the spectrum -HSD, if they fit the diagnostic criteria, unless they have hEDS, or another form of HDCT.

Author Isobel Knight has several books published by Singing Dragon Press including:
“A Guide to Living with Ehlers-Danlos Syndrome (Hypermobility-Type) – Bending without Breaking‘ (Second Edition) (2015)
“Using the Bowen Technique to Address Complex and Common Conditions” (2014) by John Wilks and Isobel Knight
Isobel is now working on an updated Edition of ‘A Guide to Living with…” and a whole new book which be known as a Handbook for Managing hEDS/HSD. News and updates about publication will be announced much closer to the time.